
Developmental dysplasia of the hip, synonymous with congenital hip dysplasia and often simplified to hip dysplasia, is one of the most commonly treated leg conditions in Paediatric Orthopaedics.
The hip joint is made up of a ball at the top of the thigh bone (femoral head) which sits within a socket in the pelvic bone (acetabulum). Hip dysplasia essentially means that the socket of the hip joint is shallow. It is a spectrum condition with complete hip dislocation at birth existing as the most severe manifestation. The mildest form is where the ball is in the socket but the socket remains shallow in adult life giving rise to painful arthritis. Early diagnosis is crucial to improve outcomes. The earlier the diagnosis, the greater the chances of success with less invasive treatment methods and the better the outcome. Diagnosis may be shortly after birth on ultrasound assessment, at walking age as a late presentation or later in adult life when mild hip dysplasia becomes symptomatic.
Hip dysplasia is very common. One in a hundred babies receive treatment for hip dysplasia. One in 500 babies is born with completely dislocated hips. The identified risk factors include.
However, up to 50% of children diagnosed with hip dysplasia may not have any of the above risk factors. Hip dysplasia is more common in girls than boys and more common in the first born child compared with later children. However these are considered soft risk factors as the vast majority of first born female babies have normal hips.
Ultrasound of a baby's hips is the best clinical tool we have for detecting hip dysplasia early. The recommendation is that a baby’s hips are scanned at 4-6 weeks of age. Ultrasound assessment undertaken in the first few days of life (especially in premature births) frequently over-diagnoses hip dysplasia. The reason is that the hips develop quite a lot in the first few weeks following birth (this is the basis for the recommendation of scanning hips between 4-6 weeks). Although a few countries practice universal ultrasound screening of all newborn babies' hips, most countries adopt selective screening based on the presence of risk factors for hip dysplasia. The main risk factors that are screened for are a family history of hip dysplasia amongst first degree relatives and breech lie towards the end of pregnancy.
Hip sonographers are usually the best operators for undertaking hip ultrasound assessment in newborns. The sonographer will usually scan the baby on their side, scanning each hip in turn. They will save an image of each hip in a defined plane, assess stability and measure the Alpha angle (used to define a threshold for treatment with <60 degrees viewed as abnormal). Alpha angle and stability are the key assessments on which a decision to treat is based. If these parameters are normal the baby can often be safely discharged from further follow up.
At American Hospital Dubai, any concerning scan is usually reviewed with the Pediatric Orthopedic Surgeon who will review the scan in real time with the sonographer. The decision of whether to treat is based on real time interpretation of the ultrasound images to ensure that dysplasia is appropriately diagnosed and treated.
In other centres, often the scan is done by the sonographer and the static images are reviewed later by a radiologist who may have difficulty interpreting the images. The report is then often passed on to the Orthopedic Surgeon to make a decision about treatment. At the American Hospital we offer the highest standard of care with a combined Sonographer – Pediatric orthopaedic Surgeon Clinic to make a decision on treatment based on real time image interpretation.
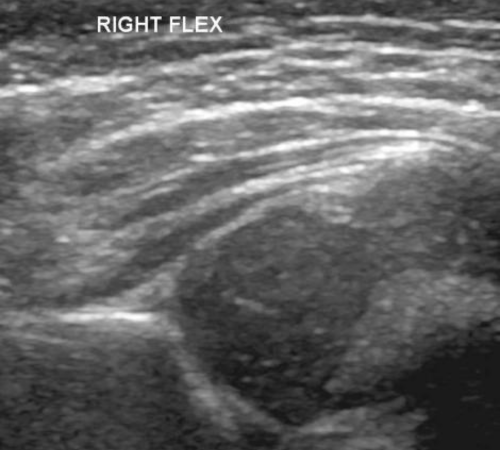
Figure 1 Ultrasound scan of a normal hip looks like a ball sitting in a socket shaped like a cup.
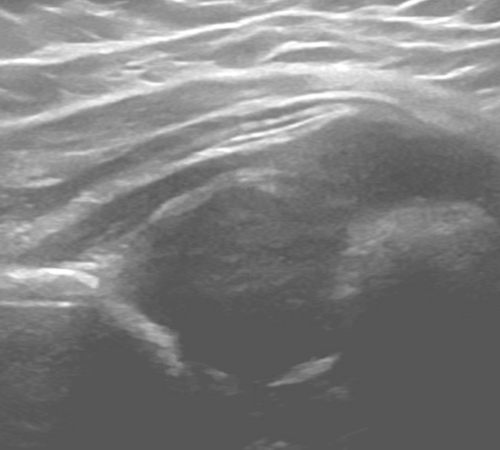
Figure 2 Ultrasound of a hip with dysplasia shows that the ball is sitting a socket that is more like a saucer.
If the scan findings are abnormal, the doctor may choose to treat your child in a Pavlik harness. Pavlik harnesses are "dynamic flexion abduction orthoses." They work best in hip dysplasia diagnosed under 6 months of age.The harness works by encouraging the baby's hips to be positioned outward at rest which is the best position of hip stability whilst permitting some movement. They are low profile and babies will sleep comfortably in them. The pavlik harnesses are usually applied and fitted by our specialised Pediatric Orthotist at American hospital Dubai and then checked by the PediatricOrthopedic Surgeon. The straps are marked so that parents know the settings when re-applying. We recommend 23 hours a day (off for 1 hour for bath and stretch) until the next visit. Appropriate sizing of the harness, adjustment of straps and looking for any complications is undertaken at each visit. The frequency of visits is based on the ultrasound findings at each visit to judge the response to treatment.
Unfortunately, not all hips respond to Pavlik harness treatment especially if the child is older when treatment is commenced. In such cases, harness treatment may be discontinued as there is a risk of damaging the femoral head through prolonged use if the hip remains dislocated. In cases where the Pavlik harness is ineffective, we would recommend arthrographic (dye injection) assessment of the hip under general anaesthetic when the child is a little older. This is usually done around the age of 6 months. The dye injection study (arthrogram) involves the injection of contrast into the hip to visualise the femoral head (usually the cartilaginous femoral head is invisible on x-ray). Once the head is visualised, we can determine where it is in relation to the socket and how easily and satisfactorily it can be placed in the socket. The arthrogram (dye study) is used to assess the hip dysplasia and whether it can be treated without open surgery. Sometimes the hip can be manually placed in to its normal position by moving the leg (closed reduction). If this is possible, the Consultant will apply a plaster cast to the child’s hips (hip spica) to keep the hips in this position allowing them to develop further. The hip spica is usually removed at 6 weeks and an arthrogram is done to assess if the hips are stable. If the hips are still unstable a further spica cast may be applied for 6 weeks.
If the hip is found to be very unstable (easily slipping in or out) or it can not be placed back into the joint in a good position, the doctor will not apply the hip spica. It is better to leave the hip free and undertake surgery when the child is older to place the hip back in. The problem with the hip being unstable is that it will come out of the joint even with the cast on. We also avoid forcing the head into the joint and applying a cast. This can cause a serious complication - avascular necrosis of the femoral head. In this complication, the femoral head is injured from the pressure of being squashed into the joint. The damage leads to the development of an abnormally shaped femoral head as the child grows older. Avascular necrosis is a serious problem for the hip and can not be reversed with surgery. A core principle of hip dysplasia treatment is to avoid causing avascular necrosis. Therefore it may be best to correct the hip dislocation with surgery rather than using a plaster cast by itself.

Fig 1. X-ray showing hip dislocation on one side. In the dislocated hip we can see that the ball has not developed into bone and is still cartilage so can not be seen on x-ray.
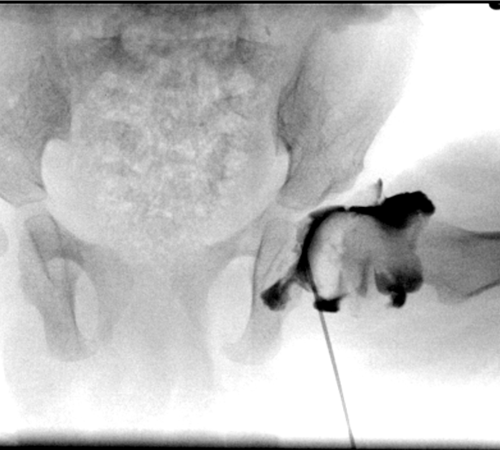
Fig 2. Arthrogram of the hip : Under x-ray guidance a needle is placed into the hip with the child under anaesthetic. Contrast dye (black) is injected into the joint to outline the ball of the hip joint (femoral head) and the relationship with the socket.

Fig 3: The hips are moved around with the child under anaesthetic to see if they dislocate. On one side the hip remains in place with a thin rim of dark dye between the ball and the socket. On the other side we can see that the ball dislocates and the empty socket fills up with dye
If your child is affected by hip dysplasia, seek a consultation with our Pediatric Orthopedic Surgeons at American Hospital Dubai for best in class care. Book an appointment now through the below links.
Patient Experience